| Key
Facts |
- Drugs toxicity
has complex pathogenesis that varies depending on the drug
- Onset of symptoms,
variable
- Radiography –
varied and nonspecific
- CT/HRCT can be
helpful for toxicity from certain drugs, e.g., amiodarone, steroids,
methysergide, mineral oil, vitamin D, talc
- Presentation: varied,
dyspnea, cough, eosinophilia
- Many have decreased
diffusing capacity
- Prognosis, variable
- Mortality from
respiratory failure
|
| Imaging
Findings |
General
Imaging findings
- Nonspecific
- Sometimes normal
CXR and abnormal CT/HRCT
- Patterns
- Pulmonary edema
- ARDS
- Fleeting peripheral
opacities (‘eosinophilic pneumonia like”)
- Granulomas
- Alveolar opacities
- Cavitation
(vasculitis)
- Interstitial
lung disease and honeycombing
- Fine calcification
- Systemic lupus
erythematosis, drug induced
- Pleural and
pericardial effusions
- Pleural effusions/fibrosis
- Hilar/mediasinal
lymphadenopathy
- Pneumothorax
(Cocaine, Nitroureas)
- Pneumomediastinum
(Cocaine)
- Pulmonary artery
hypertension (Talc, Fenfluramine)
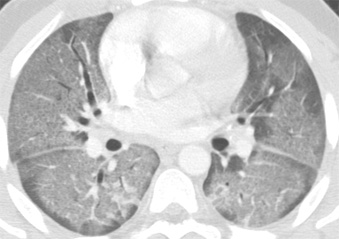
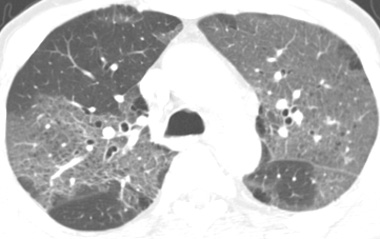
CT/HRCT
- HRCT can show early
abnormalities when radiograph is normal
- Shows distribution
of interstitial, ground glass, airspace opacities or honeycombing
- High density CT
deposits in lung and liver
- Amiodarone –
contains 37% iodine by weight
- Multiple
peripheral opacities
- Reticulonodular
opacities
- Fibrosis,
honeycombing
- Fine calcification
- Vitamin D
- CXR may be
normal
- HRCT may show
calcification before radiography
- Bone scanning
agents may show uptake
- Lipoid pneumonia
- Mineral oil
ingestion
- Low attenuation
opacities – fat density
- Micronodules, basal
predominance
- Talc
- Ground
glass opacities
- Pulmonary
artery hypertension
- Mediasinal lipomatosis/extrapleural
fat
- Steroids
- Fat attenuation
best seen with CT
|
| Differential
Diagnosis |
- Pulmonary edema,
- ARDS
- Pneumonia
- Aspiration
- UIP
- Lymphoma,
- Differentiation:
always consider history of drug use
|
| Pathological
Features |
- Pathogenesis is
complex
- Pulmonary edema
- Heroin, cocaine
- Aspirin
- Contrast media
- Cytosine arabinoside
- Mitomycin –
hemolytic uremic syndrome
- Tricyclic antidepressants
– edema, ARDS
- Hydrochlorothiazide
- Interleukin-2
- Direct toxic damage
to lung - diffuse alveolar damage
- Cytoxan, bleomycin,
methotrexate, busulfan, carmustine
- Bleomycing
- Multi
focal rounded opacities may simulate metastases
- Oxygen
- Pleura/mediastinal
fibrosis
- Methysergide
- Ergotamine
- Ergonovine
- Pleural effusions
- Methotrexate
procarcazine
- Nitrofuradantoin
- Hypersensitivity
reaction (Type I or III)
- Bleomycin,
methotrexate, procarbazine
- Neural or humoral
mechanisms
- Asthma –
propranolol, neostigmine, aspirin
- Autoimmune response,
systemic lupus erythematosis, drug-induced
- Procainamide,
hydralazine, isoniazide, phenytoin, and many other drugs
- Vasculitis
- Sulfonamides,
penicillin, cromolyn sodium
- Pulmonary hemorrhage
- Anticoagulants,
estrogens, penicillamine, and others
- Drug induced phospholipidoses
- Constrictive bronchiolitis
- Penicillamine
- Sulfasalazine
- Pulmonary calcification
- Vitamin D
- Calcium in
milk alkali syndrome
- Chronic pleural
effusions/fibrosis
- Hilar/mediasinal
lymphadenopathy
- Granulomas
- Methotraxate
- Nitrofurantoin
- Mineral oils
- Talc
|
| Clinical
Presentation |
- Age and gender,
variable
- Approximately 40
commonly used drugs may cause lung disease
- Aspirin, Mitomycin
- Methotrexate –
onset, weeks after start of treatment
- Fever, cough,
dyspnea
- Eosinophilia
- Fibrosis
- Treated with
steroids
- Mortality –
10%
- Bleomycin –
onset 3 months after start of treatment
- Diffusing capacity
most sensitive test
- With early detection
– lung disease may be reversible
- Cytosine arabinoside
– onset 2 – 21 days after start of treatment
- Recovery after
discontinuance of drug
- Some develop
respiratory failure
- ALL-TRANS Retinoic
Acid – onset 5-15 days
- Fever, respiratory
distress, anasarca, cardiac decompensation, hypotension
- Diffuse pulmonary
opacities
- Treated with
steroids
- Potentially fatal
- Amiodarone –
onset 6 months after start of treatment
- 5% incidence
of pulmonary toxicity
- Dyspnea
- Decreased diffusing
capacity
- Fatality <
20%
- Gold – onset
< 3 months after start of treatment
- Fever, proteinuria,
skin rash
- Eosinophilia
- Resolves with
discontinuation of drug
- Dilantin –
1 week – 30 years
- Rash, hepatosplenomegaly,
eosinophilia, lymphadenopathy
- Pseudolymphoma,
adenopathy, fever, skin rash, eosinophilia, hepatosplenomegaly
- Risk for lymphoma
– Hodgkin’s, nonHodgkin’s lymphoma
- Fenfluramines
- Pulmonary artery
hypertension, valvular heart disease
- Nitrofurantoin
- Acute, onset
- 1 day to 1 month after start of treatment
- Fever, chest
pain, dyspnea, rash, cough, arthralgia
- Complete
response after discontinuation of drug
- Chronic –
onset, 6 months
- Fibrosing
alveolitis
- If prolonged
exposure, may not reverse with withdrawal of drug
- 10% mortality
|
| References |
Rosenow
EC, 3rd, Myers JL, Swensen SJ, et al. Drug-induced pulmonary disease.
An update Chest 102:239-250, 1992
Rossi SE, Erasmus JJ, McAdams HP, et al. Pulmonary drug toxicity: radiologic
and pathologic manifestations Radiographics 20:1245-1259, 2000
|