| Key
Facts |
- Diffuse destructive
disorder of distal airways caused by granulomas containing Langerhans
cells
- Smoking-related
lung disease
- May present with
pneumothorax (17%) or develop recurrent pneumothoraces
- Upper and mid lung
reticulonodular opacities, sparing costophrenic angles
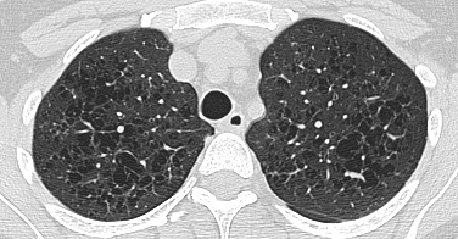
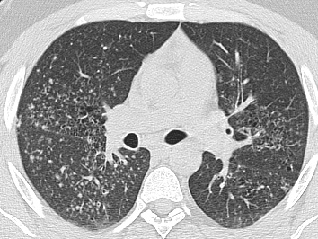
- HRCT: irregular
small nodules and bizarre shaped cysts
- Variable prognosis
|
| Imaging
Findings |
Chest
radiography
- Upper and mid lung
reticulonodular opacities, sparing costophrenic angles
- Multiple ill-defined
nodules, measuring 1-15 mm
- Cysts, honeycombing,
blebs, bullae
- Increase in lung
volume
- May see rib involvement:
lytic expansile lesion with beveled edges
- No pleural effusion
- 2/3rds of patients
eventually have resolution or stable disease
CT/HRCT
- HRCT findings may
be characteristic
- Upper and mid lung
predominance, sparing costophrenic angles
- Irregular centrilobular
nodules (usually 1- 10 mm), some cavitate
- Cysts (1–20
mm) with thin or thick walls, some lobulated, septated, or bizarre shaptes
- Ground glass opacities,
interstitial lines, septal lines
- Burned out disease
may resemble emphysema
|
| Differential
Diagnosis |
- Lympangioleiomyomatosis
(LAM)
- Differentiation
- LAM has no nodules
- Round cysts are
uniformly distributed
- Involves costophrenic
angles
- Chylothorax
|
| Pathological
Features |
- Smoking-related
lung disease (95% smoke)
- Diffuse destructive
disorder of distal airways caused by granulomas containing Langerhans
cells
- Langerhan cell
processes antigen, contains Bierbeck granule
- 1 – 15 mm
nodules (granulomas) in walls of small airways
- Nodule cavities
are due to distended airways
- Adjacent lung may
show desquamative interstitial pneumonitis (DIP) and BOOP and respiratory
bronchiolitis
- Eventually, fibrosis,
honeycombing, cysts and emphysema
- In adult, LCH most
commonly seen only in lung
- Hand-Schuller-Christian
Disease – involves lung, bone and pituitary – diabetes insipidus
(adults and adolescents)
- Letterer-Siwe –
multiorgan involvement (infants), poor prognosis
|
| Clinical
Presentation |
- Uncommon
- White adults, mostly
at ages 20 – 30, heavy smokers, males = females
- Cough, dyspnea,
chest pain, fever, weight loss, or asymptomatic (17%)
- May present with
pneumothorax (17%) or develop recurrent pneumothoraces
- Associated with
lymphoma, leukemia and solid tumors
- Diagnosis: transbronchial
lung biopsy, BAL with > 5% CD1A positive Langerhans cells, and or
HRCT. Open lung biopsy if all else fails
- Treatment
- smoking cessation,
steroids if disease is progressing
- May recur in
transplanted lung
- Variable prognosis
from complete remission to respiratory failure
- Mortality is
< 5%, worse in men, old age and in patients with recurrent pneumothoraces
|
| References |
Brauner
MW, Grenier P, Tijani K, et al. Pulmonary Langerhans cell histiocytosis:
evolution of lesions on CT scans Radiology 204:497-502, 1997
Friedman PJ, Liebow AA , Sokoloff J. Eosinophilic granuloma of lung. Clinical
aspects of primary histiocytosis in the adult Medicine (Baltimore) 60:385-396,
1981
Moore AD, Godwin JD, Muller NL, et al. Pulmonary histiocytosis X: comparison
of radiographic and CT findings Radiology 172:249-254, 1989
|